My Journey Through CBT as an Autistic/ADHD
Reflecting on my journey through Cognitive Behavioral Therapy (CBT) as someone with Autism and ADHD, I often found myself deflecting with humor during discussions of deeply traumatic experiences. When therapists inquired, “How does that make you feel?” I was frequently at a loss, grappling with alexithymia—the difficulty in identifying and articulating emotions.
When I first shared my experiences with traditional CBT as an Autistic/ADHD individual, I had no idea it would resonate so deeply with others. Across platforms, thousands of comments flooded in from people sharing similar frustrations with CBT—an approach that often fails to align with neurodivergent experiences.
From a single thread, the conversation snowballed. Readers across the globe shared how CBT left them feeling unseen, invalidated, or worse, retraumatized. This post reflects not only my story but also the collective voices of those who felt validated for the first time.
Here’s what I’ve learned—and what the response to my post has taught me.

Why Doesn’t CBT Work for Many Autistic People?
CBT (Cognitive Behavioral Therapy) is often promoted as a universal solution for mental health challenges. But for many autistic individuals, it’s like trying to force a square peg into a round hole. Why? Let’s break it down:
1. Focus on Social Norms
CBT assumes certain social norms and behaviors are universally “correct.” Forcing autistic people to align with these norms feels invalidating, dismissing the diversity of neurodivergent experiences.
“CBT assumes certain social norms and behaviors are universally correct. Forcing us autistic people to align with these norms feels invalidating. We’re not flaws to be fixed; we’re just different.”
One commenter wrote:
“I always felt like CBT was teaching me how to mask better, not how to actually process my feelings.”
2. Alexithymia: Difficulty Naming Emotions
Many autistic people, myself included, experience alexithymia—the inability to identify or describe emotions easily. When therapists ask, “How does that make you feel?” my brain often defaults to: “I don’t know; ask me in 2075.”
CBT often requires emotional articulation as a foundation for progress, making it inaccessible for those of us who struggle to name or connect with our feelings.
“CBT felt like a language I was expected to speak fluently, even though no one had ever taught me the basics,”
another commenter said.
3. Literal Thinking Styles
Autistic individuals often process information literally. CBT’s emphasis on reframing “negative” thoughts doesn’t resonate when those thoughts are grounded in tangible realities.
“‘Challenging negative thoughts’ doesn’t resonate when those thoughts are based in observable realities. Experiencing racism? That’s not a ‘negative thought’—it’s a fact.”
For many, CBT’s attempts to reframe systemic oppression or sensory overwhelm as “negativity” feel invalidating and miss the bigger picture.
4. Rigid Thought Patterns
Autistic brains are often wired with rigid thinking patterns—not as a flaw, but as an intrinsic way of processing the world. CBT’s attempts to “fix” this rigidity can feel like erasing an essential part of who we are.
One reader shared:
“CBT kept trying to tell me to ‘challenge my thoughts,’ but those thoughts were just how my brain worked. It felt like they were trying to delete me.”
What Works Better? Acceptance Over Change
CBT’s emphasis on changing thoughts and behaviors often clashes with the needs of autistic individuals. I turned to acceptance-based therapies like ACT (Acceptance and Commitment Therapy), which validated my experience instead of trying to rewrite it.
“Do I want change or acceptance? ACT allowed me to sit with my feelings instead of fighting them. It validated my experience as an autistic person.”
Thousands of commenters echoed this sentiment, sharing how therapies that emphasize acceptance, and were neuro-affirming and did not force compliance, have been life-changing for them.
Data That Speaks Volumes
It’s not just personal anecdotes—research backs this up. Studies have found that:
Over 70% of autistic adults report feeling misunderstood in traditional therapy settings.
Up to 40% of autistic adults report alexithymia, complicating CBT’s reliance on emotional identification.
Therapies like ACT have shown higher satisfaction rates among autistic individuals, especially when paired with sensory-friendly adaptations.
Sensory and Communication Barriers
1. Sensory Overload
Therapy settings can be overwhelming for autistic individuals due to sensory sensitivities. Bright lights, constant verbal exchanges, and rigid schedules can make progress nearly impossible.
2. Surface-Level Approaches
CBT often focuses on symptom management while ignoring the root causes of distress, such as systemic oppression, sensory overload, or burnout.
“I don’t need symptom management—I need therapies that address the root causes of my distress.”
This statement struck a chord with many, leading to heartfelt discussions about the need for deeper, more empathetic approaches in therapy.
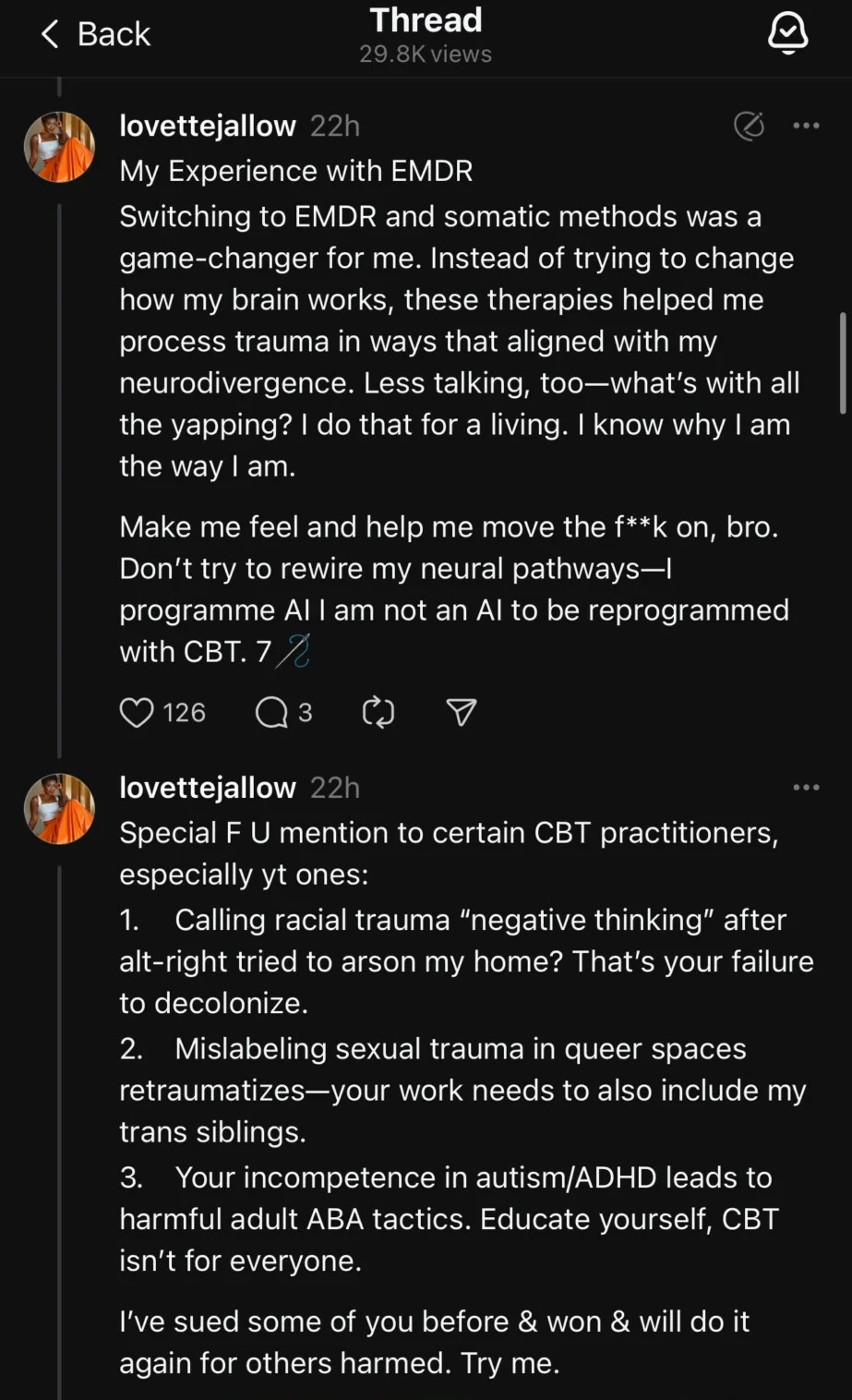
My Experience with EMDR: A Game-Changer
Switching to EMDR (Eye Movement Desensitization and Reprocessing) was transformative. Unlike CBT, it didn’t ask me to change how my brain worked. Instead, it aligned with my neurodivergence and helped me process trauma in ways that felt authentic and healing.
“EMDR isn’t about the ‘eye thing’—it’s about targeting trauma in ways that align with neurodivergence. It respects how our brains work.”
One commenter summed it up perfectly:
“EMDR allowed me to process my trauma without feeling like I had to justify or explain my brain. It was the first time I felt truly seen in therapy.”
Special Call-Outs to Certain CBT Practitioners
Not all therapy is created equal, and some CBT practitioners perpetuate harm, intentionally or not. Special mentions go to those who:
- Label racial trauma as “negative thinking.”
- Misinterpret queer trauma, retraumatizing marginalized clients.
- Use outdated ABA-like methods on autistic/ADHD adults.
As one commenter put it:
“Therapy shouldn’t feel like another battle to fight. If it does, the therapist isn’t doing their job.”
Final Thoughts
CBT didn’t work for me, and it doesn’t work for many autistic people. And that’s okay. Therapies like EMDR, ACT, and somatic methods validate who we are, offering tools for healing instead of trying to fix us.
“We don’t need to be ‘fixed.’ We need understanding, acceptance, and tools that align with how our brains and bodies work.”
To therapists: Educate yourselves. Neurodivergent people deserve spaces where we feel seen, heard, and respected—not molded to fit neurotypical expectations.
To my readers: Thank you for sharing your voices, stories, and solidarity. Together, we’re rewriting the narrative.